 Tummy Tuck (Abdominoplasty)
Tummy Tuck (Abdominoplasty)Here’s What You Need To Know About Repairing Diastasis Recti
About two-thirds of women experience diastasis recti (a.k.a. abdominal separation) after childbirth, but pregnancy isn’t the only cause. Here, The AEDITION breaks down what causes the condition and how to repair it.
New moms recovering from pregnancy and childbirth are often faced with hormonal variations, weight fluctuations, and lifestyle changes that can cause myriad physical conditions, like stretch marks, sagging skin, breast engorgement, perineum soreness, and stubborn fat pockets to name a few. While many of these heal and fade over time, some women may find that they are left with a post-pregnancy belly ‘pooch’ that leaves them wondering, why do I still look pregnant?
The answer is often a condition known as diastasis recti (a.k.a. abdominal separation), which impacts nearly two-thirds of women after childbirth — though pregnancy isn’t the only cause. Here, The AEDITION breaks down what diastasis recti is and how to repair it.
What Is Diastasis Recti?
It all begins with the linea alba (i.e. the ‘white line’ of connective tissue that runs vertically from the sternum to the pubic bone). The linea alba connects the right and left sides of the abdominal muscle wall and is visible in some individuals as the midline of the proverbial six pack. During pregnancy, hormonal changes lead to a thinning of the linea alba to accommodate the growing uterus. As the tissue thins and widens, the abdominal wall stretches and separates.
After childbirth, the majority of women are left with a condition known as diastasis recti — an ongoing separation of the left and right sides of the rectus abdominis muscles. Depending on the severity of the muscle separation, the uterus, bowels, and other internal organs may protrude, causing that so-called ‘pooch.’
Most of the time, diastasis recti resolves on its own over time. But, for some women, the abdominal separation is significant, long lasting, or both. Those who are unaware of the underlying problem may buckle down on diet and exercise without realizing that the wrong workout can worsen the condition. Many core strengthening exercises (think: sit-ups, planks, and even certain yoga poses) can exacerbate diastasis recti.
There are, however, some physical therapy techniques that may help the healing process. “A lot of stuff online is kind of gimmicky, but there is a nurse who developed a method called the Tupler Technique®,” says Beverly Hills board certified plastic and reconstructive surgeon Michael Newman, MD. “I’ve heard of people having some success with her combination of abdominal exercises performed in conjunction with a supportive garment.” Dr. Newman advises new moms — especially those who plan to have more children — to start any therapeutic exercise program as soon as they get the okay from their obstetrician.
What Happens When Diastasis Recti Doesn’t Repair Itself
For about one-third of American women, diastasis recti lingers longer than twelve months postpartum. This is more likely to occur in women who are over 35, petite, have had more than one pregnancy (or carried multiples), or have poor abdominal muscle tone to begin with. Medical history plays a role as well. Women who have had diastasis recti before or who have a history of ventral or umbilical hernia have an increased risk of developing the condition.
For many women with prolonged or severe diastasis recti, it’s much more than a cosmetic concern. The weakened abdominal and pelvic muscles can lead to difficulty exercising, lower back pain, incontinence, constipation, and painful intercourse. The tissue can also tear, causing a hernia.
Richard J. Brown, MD, a Scottsdale, Arizona-based board certified plastic and reconstructive surgeon and author of The Real Beauty Bible, recounts his experience with a thin patient who had fist-width diastasis (the condition is typically measured in finger widths). “She had what we call ‘loss of domain,’ which means that her organs — that were once packed in very tightly — expand into the bulging space, which decreases your ability to create pressure,” he explains. “Diastasis or an abdominal hernia becomes a problem when they’re so big that you get loss of domain and you start to lose some pelvic floor functions that you would normally have.”
Just as debilitating as the physical symptoms, however, are the psychological implications. Studies show that women with diastasis suffer from body image insecurities and have a lower quality of life than the general population.
Diastasis Recti Isn’t Strictly Related to Pregnancy
It is important to note that diastasis isn’t strictly a side effect of carrying and birthing a child. “If you have a ton of visceral fat, it’s like having a baby inside your stomach and that pushes out on the muscles and causes stretching,” Dr. Brown says. This means diastasis recti can happen to men, too.
Dr. Newman estimates that about five percent of his diastasis patients are male. Of his female patients, Dr. Newman figures that about 10 percent acquired the condition through massive weight gain and loss. “A lot of people come to see me because they don’t like the way their tummy looks,” he explains. “They may think they need liposuction or a tummy tuck, but we have to evaluate what’s really going on and proceed from there.”
Surgical Diastasis Recti Repair
Some patients may first visit their primary care physician to address diastasis recti. The PCP will likely then refer them to a general surgeon — though it might not be for the proper diagnosis. “They get sent to the general surgeon because it looks like a hernia, although it’s not a true hernia,” Dr. Newman says, noting that a hernia is a hole in the fascia.
Typically, a general surgeon will fix diastasis with a vertical incision down the abdomen, leaving a large scar. Alternatively, the procedure may be performed laparoscopically, using small incisions and a tiny camera — though Dr. Newman warns that the technique needs improvement. “The skin can bunch up on top, which can end up looking worse,” he cautions.
Both surgeons interviewed agree that a diastasis recti repair is best performed by a plastic surgeon. “An abdominoplasty is a nicer way to do it because you can hide the scar along the bikini line,” Dr. Newman explains, noting that about 10 percent of his diastasis patients don’t need traditional tummy tucks because they’re already fit and/or their skin is elastic enough to restore its shape post-procedure. “In patients who don’t need skin removed, you can make a smaller abdominal incision — similar to a c-section — and an incision around the belly button, without cutting any skin out,” he says. Depending on the patient, it may be possible to complete a hernia repair at the same time.
Typically, however, a diastasis repair goes hand in hand with a tummy tuck. “During a tummy tuck, when we elevate the skin flap and we’re staring at the muscles, everyone's got a gap,” says Dr. Brown. “Some have a noticeable gap; some people don’t.”
Angie*, a young mother of five, didn’t realize she had diastasis until after Dr. Brown encouraged her to lose additional weight before her tummy tuck procedure. “When the weight came off, I felt like I couldn't see the results,” she shares. “My skin kept getting saggier.” As Dr. Brown explains, no amount of weight loss can fix the physical problem of having two muscles stretched apart. They must be sewn back together, which is why diastasis recti repair is best performed by a board certified plastic surgeon.
“When it comes to diastasis, it should be a plastic surgeon repairing it, and it is a traditional tummy tuck situation,” Dr. Brown says. “Whether you take the excess skin off or not, you have to make that incision, you have to cut around the belly button just like an abdominoplasty, and you have to suture together the rectus muscles from above.”
With or without excess skin, diastasis repair is major surgery — though it’s typically performed as an outpatient procedure. “People have a lot of discomfort from the muscle tightening. It’s really debilitating to lose that core function,” Dr. Newman says. “We use a long-term anesthetic that we inject into the fascia and the muscles. It lasts for about four days, which cuts down on pain significantly and reduces the need for narcotic pain meds.” Generally, patients are up, walking, and showering the next day, he adds.
Recovering From Surgical Diastasis Recti Repair
Recovery from diastasis repair mirrors that of a tummy tuck. It usually requires two to three weeks off work, with no strenuous exercise or lifting for the first six weeks post-op. “Data shows that a scar isn’t full strength until about six weeks, and stress can break it open before then,” Dr. Brown explains. He tells patients to anticipate their recovery in stages, with most restrictions fully lifted around three to four months after the procedure. Full recovery can be expected at the 12-month mark. “It can take up to a year for the scar tissue to soften and not have any pulling or tugging,” he says.
For patients, the life-changing results are worth the wait. “The benefits far outweigh the scar,” says Angie, who is about six months post-op. “I can already feel the difference. I can feel my core support, and, with the tummy tuck, I feel like I’m 19 again. It's so worth it.”
*Patient’s name has been changed
More Related Articles
Related Procedures
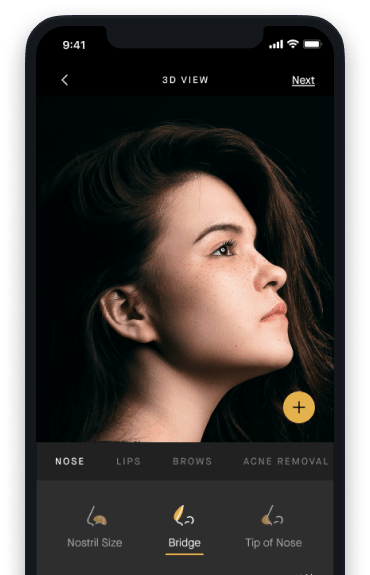
AI Plastic Surgeon™
powered by'Try on' aesthetic procedures and instantly visualize possible results with The AI Plastic Surgeon, our patented 3D aesthetic simulator.

